You’ve probably seen it in your office, chatted with the mom at the soccer field who’s lived it, or maybe… it’s your story too.
Perhaps you tried to breastfeed, and your baby seemed to want to, but something felt off.
They nursed all day (and night) long, yet never seemed satisfied.
Your nipples were shaped like lipstick after every feed, and the latch? It was painful. The kind of pain that makes you clench your toes and question everything you thought you knew about nursing.
Or maybe it’s a little later on, in the toddler years, when you start noticing other clues.
There’s drool – lots of it. Is that normal? It feels like too much.
Speech sounds a little jumbled.
Self-feeding looks like a battlefield – messy, inefficient, and every bite seems too big.
You find yourself holding your breath, worried they might choke.
Demystifying Tongue-Tie: What is it?
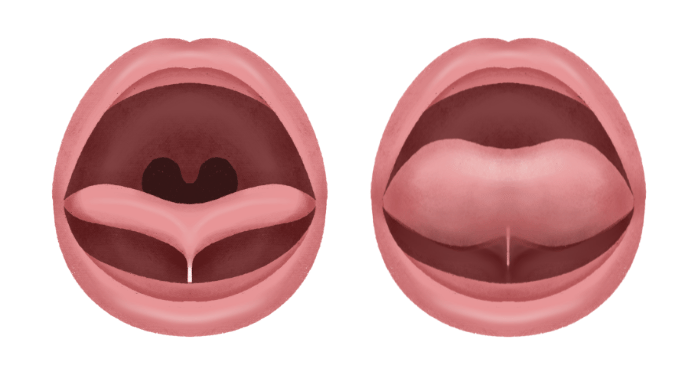
A Tongue Tie or Ankyloglossia is a thick webbing of fascia or connective tissue under the tongue that leads to symptoms and functional impact.
An anterior tie occurs when the frenulum extends to the tip of the tongue and impacts function while a posterior tie is when the frenulum inserts into the floor of the mouth posterior to the salivary glands and/or submucosal (Coryloos & Watson-Genna).
Why It Can’t Be Overlooked
Tongue ties should not be overlooked as a possible cause of dysfunction because it can lead to:
- Higher rate of tooth decay
- Sleep disordered breathing
- Digestive issues
- Myofascial tension
- Speech-articulation issues
- Malocclusion
- Chronic pain, TMD, headaches, Migraines
- Digestive issues, including chronic constipation
- Postural asymmetries
- Decreased airway patency
- Head molding or flattening
- Torticollis
- Stiff ankles, splayed toes, clenched toes
- Motor skill delay
- Clenched fists tucked thumb
- Smaller airway which can lead to bedwetting
- Snoring
- Loud breathing
- Mouth breathing
- Teeth grinding
- Reflux
How We Assess Tongue-Tie: What to Look For in the Clinic and Beyond
When it comes to assessing a tongue-tie, we have to look at both form and function.
Yes, anatomy matters – but it’s the function that tells the real story. A frenulum can look “tight,” yet function beautifully… or appear “mild,” but cause major compensations during feeding, speech, and oral rest.
Your goal as a clinician is to connect what you see with what you observe. Document, describe, and always tie your findings back to how it impacts function.
Key points to include in your assessment:
- Form: Note appearance (thin/thick, posterior/anterior), length, and tension of the frenulum.
- Function: Observe tongue mobility – can the child lift, extend, lateralize, and cup the tongue effectively?
- Feeding: Watch for latch quality, maternal discomfort, clicking sounds, loss of suction, or inefficient milk transfer/ older kiddos picky eating, big bolus size, insufficient chewing, leakage, etc.
- Speech/Oral Motor: Listen for sound distortion, tongue thrusting, or compensatory jaw/lip movements.
- Resting Posture & Breathing: Check for open-mouth posture, tongue resting low, or mouth breathing.
- Documentation: Take clear photos and videos (with consent) and include detailed descriptions in your report – visuals matter when collaborating with other professionals.
- Collaboration: Always connect the dots between your findings and referrals (ENT, IBCLC, dental, etc.).
Once you’ve identified impacts on form and function, treatment planning becomes simple. Create a tiered approach targeting the areas that were not functioning well. Part of this process and making the appropriate referrals. If nasal patency is in question, refer to and ENT. If the palate has a narrow appearance and teeth are crowded, refer to an orthodontist or airway dentist, etc. These referrals will work hand in hand with the therapy we offer to give the child a dynamic approach.
Tongue-Tie Myths vs Facts
Myth: If a child can stick out their tongue, it’s not a tongue-tie.
Fact: Sticking out the tongue is NOT an indication of if a restricted frenulum is having a functional impact on the tongue. For example, there are many individuals who can stick out their tongue but a restricted frenulum is causing a functional impact on swallowing for instance.
Myth: You can always tell if there is a tongue-tie by looking at the tongue.
Fact: You can not tell if a tongue is tied by appearance only! We must assess appearance and the overall functional impact.
Myth: A release fixes everything. Better yet- a quick snip in the Doctors office and it’s done!
Fact: A release is just one piece of the puzzle. A frenectomy addresses the structure, but the compensatory muscle movements and patterns must also be addressed through therapy before and after the release for best results.
FAQ
Does every child need a frenectomy?
No- a frenectomy should only be completed when necessary. Some children benefit from therapy alone or therapy and referral to other professionals as necessary, such a ENT, Orthodontist, etc.
What is the best age to treat a tongue-tie?
The right time to treat a tongue-tie is now! If a child has symptoms of oral dysfunction, seeking help right away can help to avoid some life-long issues that arise secondary to tongue ties.
Who should be on the care team for tongue-tie treatment?
Ideally, it’s a collaborative approach:
- IBCLC or feeding therapist to assess function and feeding patterns
- Myofunctional therapist or SLP to address oral motor (and SLP for speech) function
- ENT, dentist, or physician trained in tethered oral tissue releases
- Bodywork provider (OT, PT, CST, chiropractor) for fascia work as needed and appropriate for the patient
Are you ready to gain confidence and begin treating clients with Tongue-Tie (Ankyloglossia)? Join the Tongue Tie Bootcamp and transform your practice!


